Damaged Mitochondria and Defective Krebs cycle and ATP
production
Scientific and Medical Evidence - Listing of Research conducted worldwide section :
Severely
Damaged Mitochondria and Defective Krebs cycle and ATP production
Reduced
acyl-carnitine. Carnitine is used in mitochondria oxydation
Lowered
oxygen consumption in ME patients
Genetic markers
Scientists
in a few countries have consistently found abnormal mitochondria
degeneration and destruction and mitochondria dysfunctions in ME/CFS patients. It is worth noting that the mitochondria and the Krebs cycle are involved in ATP production and the recycling of it, and that ATP is the energy fuel of all cells, all tissues, and all organs and glands in the body. It is the fuel of the body, and governs the energy state of a person. Even minor reductions in ATP or ATP production and recycling will slow down the body and cause fatigue. Many leading medical doctors and scientists believe mitochondria dysfunction lies at the root of ME and many other illnesses involving fatigue.
The mitochondria and the Krebs cycle require essential nutrients, minerals, biochemicals, methylation end-products, SOD and glutathione in order to function effectively AND they are also susceptible to disruption / blockage / attack by viruses, bacteria, Lyme, mycoplasmas, parasites, environmental toxins, chemicals, free radicals, allergies, excess inflammation, poor detoxification status, poor antioxidant defences, lack of sleep and rest, excess metabolites (from exercise) and deprivation of the aforementioned essential nutrients. Dr. Edward Conley who runs the famous Fatigue, Fibromyalgia and Autoimmune Clinic, Michigan, USA has publically stated that solving the ATP, mitochondria and Krebs cycle problem in ME/CFS resolves the ME/CFS illness. His medical clinic has successfully treated over a thousand ME/CFS patients.
Source: Dr. Paul Cheney, The Cheney Clinic, USA.
Source: Dr. Paul Cheney, The Cheney Clinic, USA
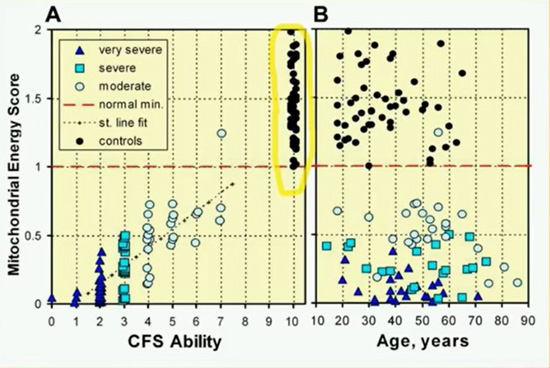
Source: Dr. Sarah Myhill. Myhill Medical Clinic, Wales.
Dr. Sarah Myhill is a distinguished and highly regarded medical doctor and researcher based in Wales. She runs the famous Myhill Clinic there. Dr. Myhill has been treating ME patients and researching the illness since the mid 1990's. Her team's collaboration with Oxford University researchers into Mitochondria has been revolutionary and provided important new medical insights into Mitochondria and their role in illness and disease. Dr. Myhill provides a scientific explanation of how mitochondria dysfunction leads to ME and CFS in the following link.
http://www.drmyhill.co.uk/wiki/CFS_-_The_Central_Cause:_Mitochondrial_Failure
The following video lecture was presented by Dr. Sarah Myhill in 2014. Her areas of speciality are the mitochondria, oxidative stress, toxins, and the immune system, and the inter-relationship between them in ME/CFS patients. She provides a brilliant analysis of these areas and provides some useful diagnostics and treatments for patients.
Tests
- Cell Metabolics
- Metabolic Features of Chronic Fatigue Syndrome. Naviaux et al. 2016
- Research by the Open Medicine Foundation in California (Dr. Ron Davis and others)
- The research papers and findings are listed on http://www.openmedicinefoundation.org
- The current findings (2016) indicate severe disruption of the citric acid cycle, inside mitochondria, the source of energy for the body. The mitochondria are functioning abnormally and not producing enough ATP. They have partially shut down and this explains the chronic exhaustion and lack of energy in patients.
- Also glucose is being converted into fatty acids not energy.
- There is deficiency of biotin.
- The GTP cyclohydrolase pathway is very low in ME/CFS, and downstream from that, as a consequence BH4 also seems to be low. This has multiple adverse effects on the human body.
- Functional impairment of pyruvate dehydrogenase (PDH), supported by increased mRNA expression of the inhibitory PDH kinases 1, 2, and 4; sirtuin 4; and PPARδ in peripheral blood mononuclear cells. Fluge et al. 2016
- According to Dr. Sarah Myhill and other medical doctors and scientific researchers the mitochondria and the Krebs cycle require essential nutrients, minerals, biochemicals, methylation end-products, SOD and glutathione in order to function effectively AND they are also susceptible to disruption / blockage / attack by viruses, bacteria, Lyme, mycoplasmas, parasites, environmental toxins, chemicals, free radicals, allergies, excess inflammation, poor detoxification status, poor antioxidant defences, lack of sleep and rest, excess metabolites (from exercise) and deprivation of the aforementioned essential nutrients
Tests recommended in research papers from 2009 and 2014, by Dr. Sarah Myhill and some other researchers from Oxford University
- Mitochondria DNA and Gene tests
These are listed in the following paper
Mitochondrial DNA variants correlate with symptoms in myalgic encephalomyelitis/chronic fatigue syndrome.
J Transl Med. 2016 Jan 20;14(1):19. doi: 10.1186/s12967-016-0771-6. Billing-Ross P1, Germain A2, Ye K3, Keinan A4, Gu Z5, Hanson MR6.
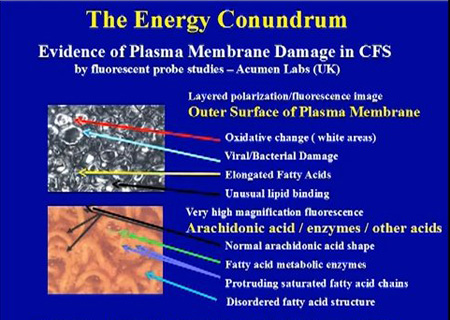
- Mitochondria Function Profile test and Micro-Respiratory studies test (Acumen Laboratory, Devon) - highly recommended by Dr. Myhill
The level of ATP in cells, and rate of ATP production and recycling in cells. Including the efficiency with which ATP is made from ADP and the level of oxidative phosphorylation. Level of mitochondria nutrients. Superoxide Dismustase and Glutathione tests and Cell free DNA test. These are all included in the Mitochondria Function Profile test and Micro-Respiratory studies test (Acumen Laboratory, Devon).
- Lactic acid levels Test
A high level of lactic acid has been found in ME patients. This has negative effects on the mitochondria and the production and release of energy.
- Translocator protein studies test - highly recommended by Dr. Myhill
Impairment of the protein which transports ATP and ADP across mitochondrial membranes. This is called the Translocator protein. Mitochondrial numbers, mitochondrial structure and mitochondrial DNA. Identify toxins blocking the three main areas (oxidative phosphorylation, translocator protein and mitochondrial DNA), and the levels of calcium, magnesium, zinc, potassium (and the pH) associated with mitochondrial membranes.
- Cardiolipin Profile test (Acumen Laboratory, Devon) - highly recommended by Dr. Myhill
This measures damage to the mitochondria membranes. This can affect mitochondria function and ATP production and transport.
Acumen Laboratory has no web site currently but can be contacted directly via email at acumenlab@hotmail.co.uk or telephone on +44 (0)7707 877175. Postal address is Acumen, PO Box 129, Tiverton, Devon EX16 0AJ, UK or through Dr. Sarah Myhill's clinic
- Mitochondrial Respiration Studies
(Acumen Laboratory)
This test can identify when oxidative phosphorylation is uncoupled from the electron transport chain. Uncoupling can be caused by toxins.
Acumen Laboratory has no web site currently but can be contacted directly via email at acumenlab@hotmail.co.uk or telephone on +44 (0)7707 877175. Postal address is Acumen, PO Box 129, Tiverton, Devon EX16 0AJ, UK or through Dr. Sarah Myhill's clinic
- Test PGC-1α levels. These determine mitochondria capabilities, the build up of lactic acid and glycosis.
- Important Cardiac and Mitochondria findings in ME and CFS
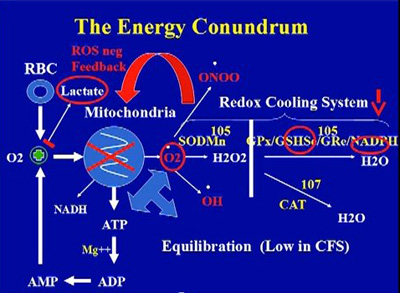
Redox Control
"All CFS cases are toxic to oxygen by echo derived IVRT response criteria as against 1/3 of healthy controls who are mildly toxic to oxygen but when probed carefully are not as healthy as they purport to be."
Dr. Paul Cheney, The Cheney Clinic, USA.
- Test for oxygen toxicity by echo derived IVRT response criteria.
- Test for poor or defective redox control. Poor redox control is found in most ME patients and is related to mitochondrial dysfunctions. It may also be responsble for low sedimentation rates due to oxidative damage to blood cells. These tests are highly recommended by Dr. Paul Cheney.
- Test for
low GSH/GSSG ratios, low NADPH, low SOD or GPx function. Dr. Cheney typically finds
low GSH/GSSG ratios, low NADPH, low SOD or GPx function in his medical practice.
- Full Intracellular Calcium Studies
(Acumen Laboratory) is highly recommended by Dr. Myhill
High calcium levels can block mitochondria functions.
Acumen Laboratory has no web site currently but can be contacted directly via email at acumenlab@hotmail.co.uk or telephone on +44 (0)7707 877175. Postal address is Acumen, PO Box 129, Tiverton, Devon EX16 0AJ, UK or through Dr. Sarah Myhill's clinic
- Toxins which block mitochonria functions and destroy mitochondria - highly recommended by Dr. Myhill
- The assessment of the energy metabolism in patients with chronic fatigue syndrome by serum fluorescence emission.
Mikirova N, Casciari J, Hunninghake R.Altern Ther Health Med. 2012 Jan-Feb;18(1):36-40.
- Glutathione Tests. Glutathione is essential for mitochondria function and protection and for detoxification
- Red Cell Glutathione Peroxidase (GSH-PX)
(Acumen)
- Red Cell Glutathione
(Acumen)
Acumen Laboratory has no web site currently but can be contacted directly via email at acumenlab@hotmail.co.uk or telephone on +44 (0)7707 877175. Postal address is Acumen, PO Box 129, Tiverton, Devon EX16 0AJ, UK or through Dr. Sarah Myhill's clinic
- Biolab tests for Vitamins and Minerals in body which are essential for Mitochondria function annd structural integrity. Vitamins A, C, D, E and B-complex, magnesium, zinc, copper, manganese, selenium, essential fatty acids.
Test Fatty acids levels. Omega 3 levels in the body are related to inflammation and cell membrane integrity (Dr. Basant Puri, Hammersmith Hospital and Imperial College London in England).
- Genetic tests for Mitochondria disorders
Courtagen offer a range of tests and are leaders in this emerging field
- Multiple Mitochondria tests
A major hospital or medical clinic may be able to do the following:
- Do biopsy of affected or inflamed muscle, and areas of inflammation in the body. Muscle tissue and blood samples.
- Test tor Mitochondria structure abnormalties. Including Mitochondria membranes damage, cristae damage, Mitochondria DNA damage, fibres fragmentation and damage, etc.
- Test for Mitochondria function abnormalities. Including Krebs cycle, ATP production and usage, electron transport chain abnormalities, etc.
- Measure levels of Malondialhehyde.
- Check for accompanying enteroviral infections and other viral / mycoplasma / Lyme / bacteria infections
which would interfere with mitochondria structure and function
- Deficient Electron Transport Chain
- Impaired Oxidative Phosphorylation
- Krebs cycle
- "We performed histochemical and quantitative analysis of enzymatic activities and studies of mitochondrial DNA deletions. All specimens showed hypotrophy, fibres fragmentation, red ragged fibres, and fatty and fibrous degeneration. Electron microscopy confirmed these alterations, showing degenerative changes, and allowed us to detect poly/pleomorphism and cristae thickening of the mitochondria. The histochemical and quantitative determination of the enzymatic activity showed important reduction, in particular of the cytochrome-oxidase and citrate-synthetase. The ‘common deletion’ of 4977 bp of the mitochondrial DNA was increased as high as 3,000 times the normal values in three patients. Our results agree with those of Behan et al 1991 and Gow et al 1994. The alterations are compatible with a myopathy of probable mitochondrial origin (which) could explain the drop in functional capability of the muscle ” (JCFS 1996:2:(2/3):76-77)
- Decreased phosphocreatine resynthesis following exercise
- Damage to mitochondrial respiratory chain in neurons
- Acceleration of glycolysis
- Reduced cerebral glucose metabolism
- Increased cerebral lactate
- Increased cerebral choline
- Reduced levels of N-acetyl aspartate
- Check ATP levels while resting, while exercising and for 24 hours and 48 hours after exercise
- Check for ADP levels and AMP levels in patient while resting, while exercising and for 24 hours and 48 hours after exercise. Are they abnormallly high ?
- Do up profile for levels of ATP, ADP, and AMP in patient while resting, while exercising and for 24 hours and 48 hours after exercise.
- Check for Purine levels in patient. while resting, while exercising and for 24 hours and 48 hours after exercise. Are they abnormallly high ?
- Check for evidence of oxidative damage to the
mitochondria while exercising and for 24 hours and 48 hours after exercise.
- Check for abnormally
high build-up of lactic acid in the cells of CFS patients while exercising and for 24 hours and 48 hours after exercise. Also check for intracellular
acidosis and extracellular alkalosis The
mitochondria are not completing the aerobic processes that
metabolise glucose, to form complete oxidation. This is contributing to the intracellular
acidosis and extracellular alkalosis found in CFS patients.
- Test for infections by cell wall deficient pathogens and co-infections such as Mycoplasmas, Lyme, Bartonella, Ehirlichia, Babesia, Brucella, Chlamydia, Enteroviruses, Herpes viruses 1-8 which have been found in patients and inflict substantial damage to the mitochondria membrane and cell membrane and joints over time.
- Nuclear magnetic resonance imaging (NMRI) techniques allow the direct measurement of mitochondrial functioning, rate of glycolysis and availability of energy. A major national hospital should be able to provide this.
- 31-P NMR spectroscopy
- Use 31P nuclear magnetic resonance spectroscopy to detect abnormal increase in the level of intracellular lactic acid
Arnold DL, Bore PJ, Radda GK, Styles P, Taylor DJ: Excessive intracellular acidosis of skeletal muscle on exercise in a patient with a post-viral exhaustion/fatigue syndrome. Lancet 1984, 1:1367-1369
- 31-P NMR spectroscopy have reported significant down regulation of oxidative phosphorylation
www.me-ireland.com/scientific/3.htm
- Ventricular cerebrospinal fluid lactate levels
Mathew SJ, Mao X, Keegan KA, Levine SM, Smith EL, Heier LA, Otcheretko V, Coplan JD, Shungu DC: Ventricular cerebrospinal fluid lactate is increased in chronic fatigue syndrome compared with generalized anxiety disorder: an in vivo 3.0 T (1)H MRS imaging study. NMR Biomed 2009, 22:251-258
Murrough JW, Mao X, Collins KA, Kelly C, Andrade G, Nestadt P, Levine SM, Mathew SJ, Shungu DC: Increased ventricular lactate in chronic fatigue syndrome measured by 1H MRS imaging at 3.0 T. II: comparison with major depressive disorder. NMR Biomed 2010, 23:643-650
- Do you eat foods containing high levels of toxins ?
- hot dogs
- sodas and fizzy drinks
- foods containing MSG
- foods containing hydrogenated fats
- foods containing saturated fats
- diet drinks containing aspartame
- sausages and cured meats containing nitrosamines
- chlorine in bathing / swimming water
- foods containing additives and flavourings with E numbers
- foods containing toxin residues from the land (arsenic in some rice)
- flouride in drinking water
- un-filtered drinking water
all of these increase toxin load on the body with adverse effects on the body, in particular the immune system, the DNA, the mitochondria, the endocrine system and the brain and nervous system. Eliminate these foods and drinks from the diet.
- 1/3 or more of the Mitochondria's DNA is missing in ME
patients. This will require specialised tests of patients.
- The cristae (the infoldings of the inner membrane of
mitochondria) have gone, leaving honeycombed patterns. This
suggests a toxic or stress phenomeon in the mitochondria.
Mitochondrial abnormalities in PVFS. ( Acta Neuropathalogica,
1991, 83, 61-65. Professor Peter Behan, The Institute of
Neurological Sciences, University of Glasgow, Scotland)
- Test for unusual pattern of mitochondrial DNA deletions in skeletal
muscle. These patterns are detailed in the following research
paper: Hum Mol Genet, 1995 April, 4(4) ), McCully (US),
Suhadolnik (US) and Brad J. Chazotte
Mitochondria nutrients, co-factors and substrates
- Reduced levels of acyl-carnitine. Carnitine is used in mitochondria
oxydation.
Carnitine is essential for mitochondria health and function.
- Kuratsune H, Yamaguti K, Lindh G, Evengard B, Takahashi M, Machii T, Matsumura K, Takaishi J, Kawata S, Langstrom B, Kanakura Y, Kitani T, Watanabe Y (1998), "Low levels of serum acylcarnitine in chronic fatigue syndrome and chronic hepatitis type C, but not seen in other diseases", Int J Mol Med. Jul;2(1):51-6
- Research papers of Professor Peter Behan, The Institute of Neurological Sciences,
University of Glasgow, Scotland)
- Kuratsune H, Yamaguti K, Takahashi M, e.a. (1994), "Acylcarnitine deficiency in chronic fatigue syndrome", Clin Infect Dis, Jan;18 Suppl 1:S62-7
- Inazu M, Matsumiya T (June 2008). "[Physiological functions of carnitine and carnitine transporters in the central nervous system]". Nihon Shinkei Seishin Yakurigaku Zasshi (in Japanese) 28 (3): 113–20. PMID 18646596
- Malaguarnera M, Gargante MP, Cristaldi E et al. (2008). "Acetyl L-carnitine (ALC) treatment in elderly patients with fatigue". Arch Gerontol Geriatr 46 (2): 181–90. doi:10.1016/j.archger.2007.03.012
- De Simone C, Famularo G, Tzantzoglou S, et al. Carnitine depletion in peripheral blood mononuclear cells from patients with AIDS: effect of oral L-carnitine. AIDS 1994;8:655-660
- Jones, M. G., Goodwin, C. S., Amjad, S. & Chalmers, R. A. Plasma and urinary carnitine and acylcarnitines in chronic fatigue syndrome. Clinica chimica acta; international journal of clinical chemistry 360, 173–7 (2005).
- Plioplys AV, Plioplys S. Serum levels of carnitine in chronic fatigue syndrome: clinical correlates. Neuropsychobiology 1995;32:132-138
- Plioplys AV, Plioplys S. Amantadine and L-carnitine treatment of chronic fatigue syndrome. Neuropsychobiology. 1997;35:16-23.
Famularo G, De Simone C. A new era for carnitine? Immunol Today 1995;16:211-2133
- Reuter, S. E. & Evans, A. M. Long-chain acylcarnitine deficiency in patients with chronic fatigue syndrome. Potential involvement of altered carnitine palmitoyltransferase-I activity. Journal of internal medicine 270, 76–84 (2011).
- Coenzyme Q10 Deficiency
- Maes M, Mihaylova I, Kubera M, Uytterhoeven M, Vrydags N, Bosmans E: Coenzyme Q10 deficiency in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is related to fatigue, autonomic and neurocognitive symptoms and is another risk factor explaining the early mortality in ME/CFS due to cardiovascular disorder. Neuro Endocrinol Lett 2009, 30:470-476.
- Judy W. Southeastern Institute of Biomedical Research, Bradenton, Florida. Presentation to the 37th Annual Meeting, American College of Nutrition, October 13, 1996.
- Vitamin E Deficiency
- Miwa K, Fujita M: Fluctuation of serum vitamin E (alpha-tocopherol) concentrations during exacerbation and remission phases in patients with chronic fatigue syndrome. Heart Vessels 2010, 25:319-323.
- Glutathione Deficiency
- Shungu DC, Weiduschat N, Murrough JW, Mao X, Pillemer S, Dyke JP, Medow MS, Natelson BH, Stewart JM, Mathew SJ: Increased ventricular lactate in chronic fatigue syndrome. III. Relationships to cortical glutathione and clinical symptoms implicate oxidative stress in disorder pathophysiology. NMR Biomed 2012, 25:1073-1087.
- Magnesium Deficiency
- Manuel y Keenoy B, Moorkens G, Vertommen J, Noe M, Neve J, De Leeuw I: Magnesium status and parameters of the oxidant-antioxidant balance in patients with chronic fatigue: effects of supplementation with magnesium. J Am Coll Nutr 2000, 19:374-382.
- Howard JM, Davies S, Hunnisett A. Magnesium and chronic fatigue syndrome. Letter. Lancet 1992;340:426.27.
- Manuel y Keenoy B, Moorkens G, Vertommen J, Noe M, Neve J, De Leeuw I: Magnesium status and parameters of the oxidant-antioxidant balance in patients with chronic fatigue: effects of supplementation with magnesium. J Am Coll Nutr 2000, 19:374-382.
- Chambers D, Bagnall AM, Hempel S, Forbes C (October 2006). "Interventions for the treatment, management and rehabilitation of patients with chronic fatigue syndrome/myalgic encephalomyelitis: an updated systematic review". J R Soc Med 99 (10): 506–20. doi:10.1258/jrsm.99.10.506. PMC 1592057
- Cox IM, Campbell MJ, Dowson D (1991). "Red blood cell magnesium and chronic fatigue syndrome". Lancet 337 (8744): 757–60. doi:10.1016/0140-6736(91)91371-Z
- Grant JE, Veldee MS, Buchwald D. Analysis of dietary intake and selected nutrient concentrations in patients with chronic fatigue syndrome. J Am Diet Assoc 1996;96:383-386
- Cox IM, Campbell MJ, Dowson D. Red blood cell magnesium and chronic fatigue syndrome. Lancet 1991;337:757-760
- Howard JM, Davies S, Hunnisett A. Magnesium and chronic fatigue syndrome. Letter.Lancet 1992;340:426.
- Jessop, Carol – reported in the Fibromyalgia Network Newsletter compendium #2, October 1990-January 1992. 53.
- Moorkens G, Manuel Y, Keenoy B, et al. Magnesium deficit in a sample of the Belgian population presenting with chronic fatigue. Magnes Res 1997;10:329-337.
- Omega-3 oils and Zinc Deficiencies
- Maes M, Mihaylova I, Leunis JC: In chronic fatigue syndrome, the decreased levels of omega-3 poly-unsaturated fatty acids are related to lowered serum zinc and defects in T cell activation. Neuro Endocrinol Lett 2005, 26:745-751.
- Chambers D, Bagnall AM, Hempel S, Forbes C (October 2006). "Interventions for the treatment, management and rehabilitation of patients with chronic fatigue syndrome/myalgic encephalomyelitis: an updated systematic review". J R Soc Med 99 (10): 506–20. doi:10.1258/jrsm.99.10.506. PMC 1592057
- Behan PO, Behan WM, Horrobin D (1990). "Effect of high doses of essential fatty acids on the postviral fatigue syndrome". Acta Neurol. Scand. 82 (3): 209–16. doi:10.1111/j.1600-0404.1990.tb04490.x
- Howard JM, Davies S, Hunnisett A. Magnesium and chronic fatigue syndrome. Letter. Lancet 1992;340:426
- Gray JB, Martinovic AM. Eicosanoids and essential fatty acid modulation in chronic disease and the chronic fatigue syndrome. Med Hypotheses 1994;43:31-42
- Kury PG, Ramwell PW, McConnell HM. The effect of prostaglandin E1 and E2 on the human erythrocyte as monitored by spin labels. Biochem Biophys Res Commun 1974;56:478-483
- Lower serum zinc in Chronic Fatigue Syndrome (CFS): relationships to immune dysfunctions and relevance for the oxidative stress status in CFS.Maes M, Mihaylova I, De Ruyter M. J Affect Disord. 2006 Feb;90(2-3):141-7. Epub 2005 Dec 9.
- Jessop, Carol – reported in the Fibromyalgia Network Newsletter compendium #2, October 1990-January 1992. 53.
- Research papers on Zinc in ME and CFS
- D-Ribose Deficiency
- Teitelbaum, J. E., Johnson, C. & St Cyr, J. The use of D-ribose in chronic fatigue syndrome and fibromyalgia: a pilot study. Journal of alternative and complementary medicine (New York, N.Y.) 12, 857–62 (2006).
- Teitelbaum, J., Jandrain, J. & McGrew, R. Treatment of Chronic Fatigue Syndrome and Fibromyalgia with D-Ribose– An Open-label, Multicenter Study. The open pain journal 32–37 (2012).
- NADH Deficiency
- Forsyth LM, Preuss HG, MacDowell AL, Chiazze L, Birkmayer GD, Bellanti JA (February 1999). "Therapeutic effects of oral NADH on the symptoms of patients with chronic fatigue syndrome". Ann. Allergy Asthma Immunol. 82 (2): 185–91.
- Santaella, M. L., Font, I. & Disdier, O. M. Comparison of oral nicotinamide adenine dinucleotide (NADH) versus conventional therapy for chronic fatigue syndrome. Puerto Rico health sciences journal 23, 89–93 (2004).
- Alegre, J. et al. Nicotinamide adenine dinucleotide (NADH) in patients with chronic fatigue syndrome. Revista clínica española 210, 284–8 (2010).
|

